Drugs Treatments for Asthma
Medication is the cornerstone of asthma treatment and the main way asthma is controlled. Asthma medications can be divided into two basic categories:
Anti-inflammatory medications, also called long-term controller medications:
Work slowly and last a long time.
Reduce the inflammation that makes the bronchial tubes overly sensitive.
Must be used on a regular basis to be effective. Those with persistent asthma will need to take anti-inflammatory medication daily.
Are considered a first line of preventive care because they help to prevent asthma attacks from starting. However, they do not immediately stop asthma attacks once they've begun.
Bronchodilators, also called quick-reliever (rescue) medications:
Work quickly and last for varying periods of time
Open narrowed airways and relieve bronchoconstriction (spasms of the airways)
Do little to reduce the chronic inflammation that makes bronchial tubes overly sensitive
Help stop asthma attacks once they've begun, and are often used on an "as-needed" basis
Your doctor will determine the type of medication that you will use based on your asthma classification. Generally, if you have intermittent asthma, you are only given quick-relief medication.
Asthma medications come in all sorts of forms -- sprays, pills, powders, liquids and shots -- and are sold under many brand names. New medications frequently come on the market.
Medications that are swallowed in pill or liquid form usually have systemic, or total body, side effects. Inhaled medications go primarily to the lungs, decreasing the overall side effects. Medications vary as to "onset of action," or the amount of time it takes to feel the results. Another variable is when the peak, or maximal effect, occurs.
Control medications (anti-inflammatory medications)
Once asthma has been diagnosed, many patients start on controller medicine, also called long-term preventative medication or maintenance medication.
Types of long-term control medications include inhaled corticosteroids cromolyn sodium and nedocromil sodium and long-acting beta-agonists (beta-adrenergic agonists).
Corticosteroids
Inhaled corticosteroids are the most effective medications to prevent swelling and irritation in the lining of inflamed airways. Dry powder or aerosol are the commonly prescribed forms.
Inhaled corticosteroids are used as daily controller medications in those with persistent asthma. They are a type of steroid medication that is related to cortisone, a hormone produced naturally by the adrenal glands. They block the chemicals in your body that cause inflammation and can take a week or more to start working fully.
Patients switching from an oral steroid like prednisone, to an inhaled steroid need to be careful. While adjusting to the switch, one may not be able to handle major stress such as surgery or severe infection or trauma without additional systemic steroid. Discuss with your health care provider.
Brand Name Generic Name
Beclovent®
Vanceril®
Vanceril DS®
QVAR® beclomethasone
dipropionate
Beclomethasone
Pulmicort Turbuhaler® Budesonide
AeroBid®
AeroBid®-M Flunisolide
Flovent®
Flovent Rotadisk® fluticasone propionate
Azmacort® triamcinalone acetonide
If taken as directed, inhaled corticosteroids do not cause the potentially serious side effects that can occur with the regular use of oral corticosteroids. Still, inhaled corticosteroids do have side effects (as does any medication): hoarseness can occur with increasing dosages and vocal stress; thrush (a yeast infection in the mouth) and mouth irritations are the most common.
Women who take large doses of inhaled corticosteroids because of severe asthma may experience bone density loss after menopause. In the New England Journal of Medicine, researchers reported an increased risk of glaucoma formation with older adults using inhaled corticosteroids.
In addition, there has been some concern regarding possible growth retardation in children, which appeared to be dose related: The longer corticosteroids are used and the higher the dosage, the more likely growth stunting is to occur.
Cromolyn sodium and nedocromil sodium
These medicines reduce inflammation by preventing the activation of messages in your body that tell the immune system to start acting up. They are less effective than inhaled steroids.
Cromolyn sodium and nedocromil sodium are typically used as daily controller medications, but can also be used before exercise or exposure to an allergic asthma trigger.
Brand Name Generic Name
Intal® sodium cromoglycate
Tilade® nedocromil sodium
Long-acting beta-agonist inhaler (beta-adrenergic agonist)
This medication prevents constriction by stimulating the messages to the smooth muscles in the airways that help relax the bronchial tubes. Long-acting beta-agonists are often used as a long-term control medication in moderate persistent or severe persistent asthma, particularly to prevent symptoms for those with nighttime symptoms and/or exercise-induced asthma.
Brand Name Generic Name
Foradil® Formoterol
Serevent® Salmeterol
Methylxanthines
This type of oral medication is a bronchodilator. Theophylline is rarely used in asthma treatment today and is noted for significant side effects, including nervousness, hyperactivity, upset stomach, and headaches. Tell your doctor if you are taking any other medicine with theophylline because side effects may occur.
Leukotriene modifiers
Antileukotrienes, also known as leukotriene inhibitors or modifiers, are among the newest oral anti-inflammatory medications. The body processes leukotrienes, chemicals that cause inflammation, as part of the reaction to an allergen. They may be useful as a primary treatment to control mild persistent asthma or as add-on therapy with moderate or severe persistent asthma.
All three drugs block the recognition of allergens, thereby avoiding the usual cascade of symptoms. The result is a decrease in the frequency of asthma flare-ups and a decreased need for quick-relief medications.
Brand Name Generic Name
Accolate® Zafirlukast
Zyflo® Zileuton
Singulair® Montelukast
Quick-relief medications/bronchodilators
Called quick-relievers or rescue medicine, this type of medication works quickly to relieve flare-ups of asthma symptoms. They can "rescue" you and keep symptoms from getting worse.
Relievers work by opening airways and increasing airflow. They will stop the coughing, chest tightness, shortness of breath and wheezing associated with an asthma attack within 30 minutes.
Quick-relief medication is not meant to be used daily. Relievers are used at the moment you are having a flare-up of symptoms. No matter how light or severe your asthma is, your doctor will make sure that you have a reliever medication available.
Anticholinergics
Anticholinergics relax muscles around the airways to reverse airway narrowing and stop spasms in the bronchial muscles. Inhaled anticholinergics are generally not used as a first-line reliever medication for most patients with asthma as they may take several hours to take effect.
Brand Name Generic Name
Atrovent® ipratropium bromide
Combivent® ipratropium bromide and albuterol
Short-acting beta-agonists
Beta2-agonists, or short-acting beta-agonists, are the most effective bronchodilators. When bronchial muscles tighten, the airway is narrowed and asthma symptoms occur. B2-agonists work rapidly and selectively on the B2 receptors in the muscles that surround the bronchial tubes to open the airways and improve breathing by reversing bronchoconstriction, allowing the muscles to relax.
B2-agonists are generally used on an as-needed basis during an asthma episode or prior to exercise for EIA. They are not intended for use every day, more than three times in any given day, or in excess of one canister per month. Excessive use indicates poor control and the need to add or increase long-term control medications.
Brand Name Generic Name
Proventil®
Ventolin® Albuterol
Alupent® Metaproterenol
Maxair® Pirbuterol
Combination therapy
The first combination anti-inflammatory and bronchodilator, fluticasone propionate and salmeterol inhalation powder, (Advair®, Diskus®) became available in the United States in 2001. The drug does not replace fast-acting inhalers for sudden symptoms.
Other Treatments
Allergy desensitization shots
Certain sufferers of allergic asthma cannot easily control symptoms by avoiding triggers and using medication. In these cases, immunotherapy (allergy desensitization shots) may offer relief and even help prevent development of airway inflammation, resulting in chronic airway sensitivity.
According to the American Academy of Allergy, Asthma and Immunology (AAAAI), allergen immunotherapy works like a vaccination. Through exposure to small, injected amounts of a particular allergen, in gradually increasing doses, your body builds up immunity to the allergen(s) triggering an allergic reaction.
Immunotherapy appears to work best for allergies to pollen, mold, cat dander, insect stings, and dust mites. Potential side effects during treatment, according to the AAAAI, may include swelling at the site of the injection, and in rare instances, a more serious allergic reaction, resulting in asthma symptoms or an anaphylactic reaction.
Anti-IgE
Omalizumab (Xolair®) is the first biotechnology product to treat patients with a type of asthma that is related to allergies.
the A to Z directory of dealing with Health Problems & Self Care Strategies for natural remedies to your health issues.

Subscribe to get your weekly "Health Success Magazine" with a new complete & comprehensive Health Report in every edition!

to “Your Health Success”
our weekly F’R’E’E’ Newsletter
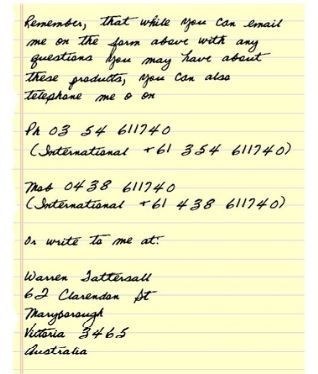
If you would like a free no-obligation private consultation or to contact Warren Tattersall for more information, please click here >> Contact Us
Click the books above to learn more about how we treat CFS naturally, to get your life back!
You will find many assorted Health Reports available for download free to you on this website!
Our free Health Success Reports are each available for you to download when you subscribe to receive them and their 7 part eCourse.
You can unsubscribe at any time, but we are sure you will want to receive all the email lessons of these informative ecourses.
Read more HERE to select the REPORT subjects of most interest (or concern) to you.