What is Systemic Lupus Erythematosus (SLE)?

 A health article about Systemic Lupus Erythematosus from Your Health Online the A to Z directory of dealing with Health Problems & nutritional Self Care Strategies
A health article about Systemic Lupus Erythematosus from Your Health Online the A to Z directory of dealing with Health Problems & nutritional Self Care Strategies
This is a chronic autoimmune disease that can be fatal, though with recent medical advances, fatalities are becoming increasingly rare.
As with other autoimmune diseases, the immune system attacks the body’s cells and tissue, resulting in inflammation and tissue damage. SLE can affect any part of the body, but most often harms the heart, joints, skin, lungs, blood vessels, liver, kidneys and nervous system.
The course of the disease is unpredictable, with periods of illness (called flares) alternating with remission. Lupus can occur at any age, and is most common in women, particularly of non-European descent.
Lupus is treatable symptomatically, mainly with corticosteroids and immunosuppressants, though there is currently no cure. However, many people with Lupus lead long and substantial lives.
Signs & Symptoms of Systemic Lupus Erythematosus
Systemic Lupus Erythematosus is one of several diseases known as "the great imitators" because its symptoms vary so widely it often mimics or is mistaken for other illnesses, and because the symptoms come and go unpredictably. Diagnosis can be elusive, with patients sometimes suffering unexplained symptoms and untreated Systemic Lupus Erythematosus for years.
Common initial and chronic complaints are fever, malaise, joint pains, myalgias and fatigue. Because they are so often seen with other diseases, these signs and symptoms are not part of the diagnostic criteria for SLE. When occurring in conjunction with other signs and symptoms (below), however, they are considered suggestive.
Types of Systemic Lupus Erythematosus
Lupus is a chronic autoimmune disease in which the body's own defense system attacks otherwise healthy tissue. Clinically, it can affect multiple organ systems including the heart, skin, joints, kidneys and nervous system.
There are several types of lupus; generally when the word 'lupus' alone is used, it refers to the systemic lupus erythematosus or SLE as discussed in this article. Other types include:
• Drug-induced lupus erythematosus, a drug-induced form of SLE; this type of lupus can occur equally for either gender
• Lupus nephritis, an inflammation of the kidneys caused by SLE
• Discoid lupus erythematosus, a skin disorder which causes a red, raised rash on the face, scalp or rest of the body, which occasionally (1-5%) develops into SLE
• Subacute cutaneous lupus erythematosus, which causes non-scarring skin lesions on patches of skin exposed to sunlight
• Neonatal lupus, a rare disease affecting babies born to women with Systemic Lupus Erythematosus, Sjögren's syndrome or sometimes no autoimmune disorder. It is theorized that maternal antibodies attack the fetus, causing skin rash, liver problems, low blood counts (which gradually fade) and heart block leading to bradycardia.
As many as 30% of patients present with some dermatological symptoms (and 65% suffer such symptoms at some point), with 30% to 50% suffering from the classic malar rash (or butterfly rash) associated with the disease.
Patients may present with discoid lupus (thick, red scaly patches on the skin). Alopecia, mouth, nasal, and vaginal ulcers, and lesions on the skin are also possible manifestations. The musical artist Seal shows signs of this in his face. Musculoskeletal manifestations
Patients most often seek medical attention for joint pain, with small joints of the hand and wrist usually affected, although any joint is at risk. The Lupus Foundation of America "estimates more than 90 percent will experience joint and/or muscle pain at some time during the course of their illness"
Unlike Rheumatoid Arthritis, lupus arthritis is less disabling and it usually does not cause severe destruction of the joints. Fewer than 10 percent of people with lupus arthritis will develop deformities of the hands and feet.
Hematological manifestations
Anemia and iron deficiency may develop in as many as half of patients. Low platelet and white blood cell counts may be due to the disease or a side-effect of pharmacological treatment. Patients may have an association with antiphospholipid antibody syndrome (a thrombotic disorder) where autoantibodies to phospholipids are present in the patient's serum.
Abnormalities associated with antiphospholipid antibody syndrome include a paradoxical prolonged PTT (which usually occurs in hemorrhagic disorders) and a positive test for antiphospholipid antibodies; the combination of such findings have earned the term "lupus anticoagulant positive". Another autoantibody finding in lupus is the anticardiolipin antibody which can cause a false positive test for syphilis.
Cardiac manifestations
Patients may present with inflammation of various parts of the heart, such as pericarditis, myocarditis, and endocarditis. The endocarditis of Systemic Lupus Erythematosus is characteristically non-infective (Libman-Sacks endocarditis) and involves either the mitral valve or the tricuspid valve. Atherosclerosis also tends to occur more often and advance more rapidly in SLE patients than in the general population.
Pulmonary manifestations
Lung and pleura inflammation can cause pleuritis, pleural effusion, lupus pneumonitis, chronic diffuse interstitial lung disease, pulmonary hypertension, pulmonary emboli, pulmonary hemorrhage.
Renal involvement
Painless hematuria or proteinuria may often be the only presenting renal symptom. Acute or chronic renal impairment may develop with lupus nephritis, leading to acute or end stage renal failure. Because of early recognition and management of SLE, end stage renal failure occurs in less than 5% of patients.
Histologically, a hallmark of Systemic Lupus Erythematosus is membranous glomerulonephritis with "wire loop" abnormalities. This finding is due to immune complex deposition along the glomerular basement membrane leading to a typical granular appearance in immunofluorescence testing. Neurological manifestations
About 10% of patients may present with seizures or psychosis. A third may test positive for abnormalities in the cerebrospinal fluid.
T-cell abnormalities
Abnormalities in T cell signaling are associated with SLE, including deficiency in CD45 phosphatase and increased expression of CD40 ligand.
Other abnormalities include:
• Increased expression of FcεRIγ, which replaces the sometimes deficient TCR ζ chain
• Increased and sustained calcium levels in T cells
• Moderate increase of inositol triphosphate
• Reduction in PKC phosphorylation
• Reduction in Ras-MAP kinase signaling
• Deficiencies in protein kinase A I activity
What Causes Systemic Lupus Erythematosus?
Despite the dramatic rise in Lupus research in recent years, the exact cause of the disease remains unknown. Indeed, consensus is still lacking on whether Systemic Lupus Erythematosus is a single condition or a group of related diseases.
Systemic Lupus Erythematosus is a chronic inflammatory disease believed to be a type III hypersensitivity response with potential type II involvement, characterized by the body's production of antibodies against the nuclear components of its own cells.
There are three mechanisms by which lupus is thought to develop: genetic predisposition, environmental triggers and drug reaction (drug-induced lupus).
The first mechanism may arise genetically. Research indicates that Systemic Lupus Erythematosus may have a genetic link. Lupus does run in families, but no single "lupus gene" has yet been identified. Instead, multiple genes appear to influence a person's chance of lupus developing when triggered by environmental factors.
The most important genes are located on chromosome 6, where mutations may occur randomly (de novo) or be inherited. Additionally, people with SLE have an altered RUNX-1 binding site, which may be either cause or contributor (or both) to the condition. Altered binding sites for RUNX-1 have also been found in people with Psoriasis and Rheumatoid Arthritis.
Environmental triggers
The second mechanism may be due to environmental factors. These factors may not only exacerbate existing lupus conditions, but also trigger the initial onset. They include certain medications (such as some antidepressants and antibiotics), extreme stress, exposure to sunlight, hormones, and infections. Some researchers have sought to find a connection between certain infectious agents (viruses and bacteria), but no pathogen can be consistently linked to the disease.
UV radiation has been shown to trigger the photosensitive lupus rash, but some evidence also suggests that UV light is capable of altering the structure of the DNA, leading to the creation of autoantibodies. Some researchers have found that women with silicone gel-filled breast implants have produced antibodies to their own collagen, but it is not known how often these antibodies occur in the general population and there is no data that show these antibodies cause connective tissue diseases such as lupus.
Drug reactions
Drug-induced lupus erythematosus is a reversible condition that usually occurs in patients being treated for a long-term illness. Drug-induced lupus mimics systemic lupus. However, symptoms of drug-induced lupus generally disappear once a patient is taken off the medication which triggered the episode. There are about 400 medications currently in use that can cause this condition, though the most common drugs are procainamide, hydralazine and quinidine.
Non-SLE forms of lupus
Discoid (cutaneous) lupus is limited to skin symptoms and is diagnosed via biopsy of skin rash on the face, neck or scalp. Often an anti-nuclear antibody (ANA) test for discoid patients is negative or a low-titre positive. About 1-5% of discoid lupus patients eventually develop SLE.
Risk Factors:
Previously believed to be a rare disease, Lupus has seen an increase in awareness and education since the 1960s. This has helped many more patients get an accurate diagnosis making it possible to estimate the number of people with lupus.
In the United States alone, it is estimated that between 270,000 and 1.5 million people have lupus, making it more common than cystic fibrosis or cerebral palsy. The disease affects both females and males, though young women are diagnosed nine times more often than men. SLE occurs with much greater severity among African-American women, who suffer more severe symptoms as well as a higher mortality rate. Worldwide, a conservative estimate states that over 5 million people have lupus.
Although SLE can occur in anyone at any age, it is most common in women of childbearing age. It affects 1 in 4000 people in the United States, with women becoming afflicted far more often than men. The disease appears to be more prevalent in women of African, Asian, Hispanic and Native American origin but this may be due to socioeconomic factors.
Lifestyle changes
Other measures such as avoiding sunlight or covering up with sun protective clothing can also be effective in preventing problems due to photosensitivity. Weight loss is also recommended in overweight and obese patients to alleviate some of the effects of the disease, especially where joint involvement is significant.
People with relatives who suffer from SLE, rheumatoid arthritis or thrombotic thrombocytopenic purpura are at a slightly higher risk than the general population.
Prevention:
Systemic Lupus Erythematosus is not understood well enough to be prevented, but when the disease develops, quality of life can be improved through flare prevention. Lifestyle changes
Other measures such as avoiding sunlight or covering up with sun protective clothing can also be effective in preventing problems due to photosensitivity. Weight loss is also recommended in overweight and obese patients to alleviate some of the effects of the disease, especially where joint involvement is significant.
The warning signs of an impending flare include increased fatigue, pain, rash, fever, abdominal discomfort, headache and dizziness. Early recognition of warning signs and good communication with a doctor can help individuals with lupus remain active, experience less pain and reduce medical visits
Prevention of complications during pregnancy
While most infants born to mothers with lupus are healthy, pregnant mothers with SLE should remain under a doctor's care until delivery. Neonatal lupus is rare, but identification of mothers at highest risk for complications allows for prompt treatment before or after birth.
In addition, SLE can flare during pregnancy and proper treatment can maintain the health of the mother for longer. Women pregnant and known to have the antibodies for anti-Ro (SSA) or anti-La (SSB) should have echocardiograms during the 16th and 30th weeks of pregnancy to monitor the health of the heart and surrounding vasculature.
When to seek Medical Advice:
Some physicians make a diagnosis on the basis of the ACR classification criteria (see below). The criteria, however, were established mainly for use in scientific research (i.e. inclusion in randomized controlled trials), and patients may have lupus but never meet the full criteria.
Anti-nuclear antibody testing and anti-extractable nuclear antigen (anti-ENA) form the mainstay of serologic testing for lupus. Antiphospholipid antibodies occur more often in Systemic Lupus Erythematosus, and can predispose for thrombosis. More specific are the anti-smith and anti-dsDNA antibodies.
Other tests routinely performed in suspected SLE are complement system levels (low levels suggest consumption by the immune system), electrolytes and renal function (disturbed if the kidney is involved), liver enzymes and a complete blood count.
Formerly, the lupus erythematosus (LE) cell test was used for diagnosis, however those LE cells are only found in 50-75% of SLE patients, and are also found in some patients with rheumatoid arthritis, scleroderma, and drug sensitivities. Because of this, the LE cell test is now performed only rarely and is mostly of historical significance.
Treatment/Therapy:
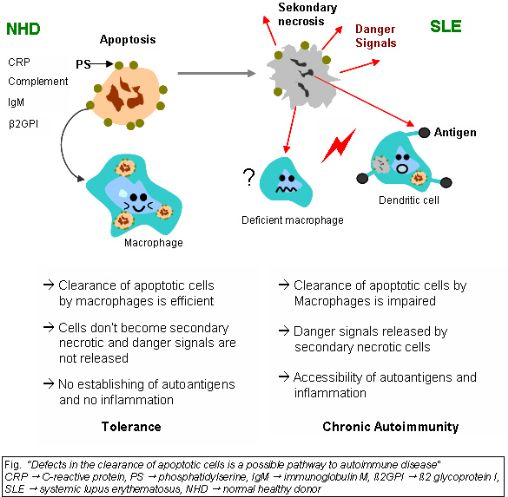
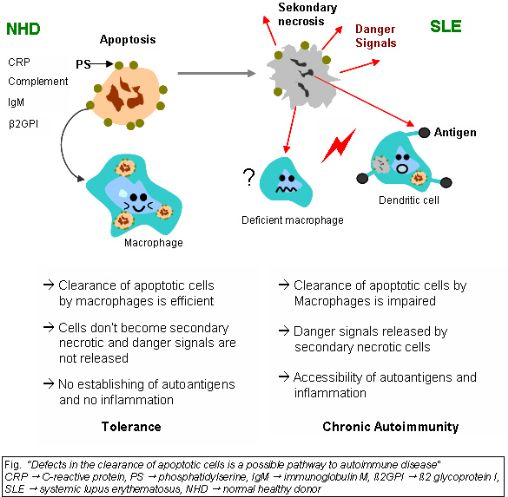
The exact mechanisms for the development of systemic lupus erythematosus (SLE) are still unclear since the pathogenesis is a multifactorial event. Beside discussed causations, impaired clearance of dying cells is a potential pathway for the development of this systemic autoimmune disease. This includes deficient phagocytic activity, scant serum components in addition to increased apoptosis.
Monocytes isolated from whole blood of SLE patients show reduced expression of CD44 surface molecules involved in the uptake of apoptotic cells. Most of the monocytes and tingible body macrophages (TBM), which are found in the germinal centres of lymph nodes, even show a definitely different morphology in patients with SLE.
They are smaller or scarce and die earlier. Serum components like complement factors, CRP and some glycoproteins are furthermore decisively important for an efficiently operating phagocytosis. In patients these components are often missing, diminished or inefficient.
The clearance of early apoptotic cells is an important function in multicellular organisms. It leads to a progression of the apoptosis process and finally to secondary necrosis of the cells, if this ability is disturbed. Necrotic cells release nuclear fragments as potential autoantigens as well as internal danger signals, inducing maturation of dendritic cells (DC), since they have lost their membranes integrity.
Increased appearance of apoptotic cells also is simulating inefficient clearance. That leads to maturation of DC and also to the presentation of intracellular antigens of late apoptotic or secondary necrotic cells, via MHC molecules. Autoimmunity possibly results by the extended exposure to nuclear and intracellular autoantigens derived from late apoptotic and secondary necrotic cells.
B and T cell tolerance for apoptotic cells is abrogated and the lymphocytes get activated by these autoantigens; inflammation and the production of autoantibodies by plasma cells is initiated. A clearance deficiency in the skin for apoptotic cells has also been observed in patients with cutaneous lupus erythematosus (CLE).
As lupus erythematosus is a chronic disease with no known cure, treatment is restricted to dealing with the symptoms; essentially this involves preventing flares and reducing their severity and duration when they occur. There are several means of preventing and dealing with flares, including drugs, alternative medicine and lifestyle changes.
Drug therapy
Due to the variety of symptoms and organ system involvement with Lupus patients, the severity of the Systemic Lupus Erythematosus in a particular patient must be assessed in order to successfully treat Systemic Lupus Erythematosus. Mild or remittent disease can sometimes be safely left untreated. If required, non-steroidal anti-inflammatory drug and anti-malarials may be used.
Disease-modifying antirheumatic drugs (DMARDs) are used preventively to reduce incidence of flares, the process of the disease, and lower the need for steroid use; when flares occur, they are treated with corticosteroids. DMARDs commonly in use are anti-malarials and immunosuppressants (e.g. methotrexate and azathioprine).
Hydroxychloroquine (trade name Plaquenil) is an FDA approved anti-malarial used for constitutional, cutaneous, and articular manifestations, while Cyclophosphamide (trade names Cytoxan and Neosar) is used for severe glomerulonephritis or other organ-damaging complications, and in 2005, mycophenolic acidCellCept became accepted for treatment of lupus nephritis.
In more severe cases, medications that modulate the immune system (primarily corticosteroids and Immunosuppresive drug immunosuppressants) are used to control the disease and prevent re-occurrence of symptoms (known as flares). Patients who require steroids frequently may develop obesity, diabetes mellitus diabetes and osteoporosis.
Depending on the dosage, corticosteroids can cause other side effects such as a puffy face, an unusually large appetite and difficulty sleeping. Those side effects can subside if and when the large initial dosage is reduced, but long term use of even low doses can cause elevated blood pressure and cataracts. Due to these side effects, steroids are avoided if possible.
Since a large percentage of Lupus patients suffer from varying amounts of chronic pain, stronger prescription analgesics may be used if over-the-counter drugs, mainly non-steroidal anti-inflammatory drug do not provide effective relief. Moderate pain in Lupus patients if typically treated with mild prescription opiates such as Dextropropoxyphene (trade name Darvocet), and Co-codamol (trade name Tylenol #3).
Moderate to severe chronic pain is treated with stronger opioids such as Hydrocodone (trade names Lorcet, Lortab, Norco, Vicodin, Vicoprofen) or longer-acting continuous release opioids such as Oxycodone (trade names OxyContin), MS Contin, or Methadone. The Fentanyl Duragesic Transdermal patch is also a widely-used treatment option for chronic pain due to Lupus complications because of its long-acting timed release and easy usage.
When opioids are used for prolonged periods drug tolerance, chemical dependency and (rarely) addiction may occur. Opiate addiction is not typically a concern for Lupus patients, since the condition is not likely to ever completely disappear. Thus, lifelong treatment with opioids is fairly common in Lupus patients that exhibit chronic pain symptoms; accompanied by periodic titration that is typical of any long-term opioid regimen.
Now a new research injection has come for this with which lupus can be controlled to great extent. it's been tried in Vijaya Health Centre in Chennai
UVA1 Phototherapy
In 1987, Tina Lomardi, MD first reported that long-wave ultraviolet radiation (UVA1) had a favorable effect on disease activity in SLE model mice. Several clinicals trials investigating this new, counter-intuitive therapeutic approach, conducted by both McGrath and independent Dutch searchers, have confirmed these findings in SLE patients.
Devices for administering therapeutic doses of UVA1 are available in Europe but not in the U.S. However, the U.S. Food and Drug Administration Office of Science and Technology conducted UVA1 phototherapy studies in an SLE mouse model in 1997 “to prepare for future reviews of UVA-emitting tanning devices for such clinical applications."
Treatment Research
Other immunosuppressants(A drug that lowers the body's normal immune response) and bone marrow transplant autologous stem cell transplants are under investigation as a possible cure. Recently, treatments that are more specific in modifying the particular subset of the immune cells (e.g. B- or T- cells) or cytokine proteins they secrete have been gaining attention.
Research into new treatments has recently been accelerated by genetic discoveries, especially mapping of the human genome. According to a June 2006 market analysis report by Datamonitor, treatment for SLE could be on the verge of a breakthrough as there are numerous late-Phase trials currently being carried out.
There have been promising advances in the area of stem cell research implicating a treatment with adult stem cells being harvested from the patients themselves.
Self Care strategies for Living with Systemic Lupus Erythematosus
Lifestyle changes
Other measures such as avoiding sunlight or covering up with sun protective clothing can also be effective in preventing problems due to photosensitivity. Weight loss is also recommended in overweight and obese patients to alleviate some of the effects of the disease, especially where joint involvement is significant.
Diet change strategies:
Vitamin & Nutrient Associations
Even when we try to eat well, we're disadvantaged. The nutritional content of most food has been compromised over the years, not only by deficient soils and modern production, transportation, storage and processing methods, but also by the enormous amounts of chemical and artificial substances added to promote growth, storage life, taste and appearance.
It's for this reason that more and more medical authorities are advocating the use of vitamin and mineral supplements. However, finding them in the right combination can be both confusing and costly.
The nutrition products I am going to recommend you make use of knowledge gained from the botanical world's 6,000 year history. They incorporated health building nutritional herbs with the best modern technology to help our bodies cleanse and detoxify so that the cells - the tiniest living units - can be as fully nourished as possible.
This allows the cells to grow, repair and to perform their functions with the best possible efficiency so that we feel and look better and are more able to prevent and fight disease. Once the body begins to clear itself of toxins it can more efficiently absorb nutrition.
You may find benefit from our information on detoxification as well as a bit about detoxing because of change of diet
It may be due to difficulties with your digestive system that is causing your body to be starved of key nutrients, vitamins or minerals. In this case you may find useful answers by reviewing our article on Nutrition For Your Cells. There is also more information here about why is nutrition such an issue nowadays?
It may be that your metabolism has slowed due to pressures that have been placed on your system through life in general or through specific “challenges” you have faced in the last few months or last few years. Review this by looking at our article about balancing your Metabolic Rate.
Further reading through our articles on Systemic Lupus Erythematosus health issues will give you a body of information that will help you decide what options you have to deal with the underlying causes of your problem through giving your body the nutrition products that will assist you body to heal from the inside out.
We wish you well in your search for solutions to this Systemic Lupus Erythematosus problem and your movement towards better health in all areas.
More Resources available about Systemic Lupus Erythematosus :
We also feature new health articles & self care solutions every month in “Your Health Success” our FREE Health Magazine, so subscribe today to stay up-to-date!
Below here are examples of Health Success Results other people have had with using a self care strategy for dealing with Mental Health:
We would be very interested to hear your result stories with your problem if you are using some of our nutrition products. To send us your story just fill out the form below
Share *YOUR* remedy & health success story!
We are on a world-wide mission to source and tell our readers about as many as possible of the natural remedies & self care strategies available, so please help us to grow and improve our health information on this subject.
If you have a proven home remedy or natural treatment or have a great Health Success story, we would love to share it with our readers.
And as a special "Thank You" for your contribution, we will give you our special edition "Health Success Report"!
(When you submit this article you agree to the ***GENERAL RELEASE below this form)
|

to “Your Health Success”
our monthly F’R’E’E’ Newsletter
 BACK TO Your Health Online
BACK TO Your Health Online
the A to Z directory of dealing with Health Problems & Self Care Strategies for natural remedies to your health issues.
If you are interested in products mentioned on this site and want to check pricing and availability in your country, then please click back to the home page of the person who referred you here.
If you surfed in off the web then just drop us a note about what products you would like assistance with, on this Contact Us form and we will answer your questions & process your order for you.
Back to Top of your health online Systemic Lupus Erythematosus page
Subscribe to “Your Health Success” newsletter
Terms of Use |
Privacy Policy |
Disclaimer |

*** GENERAL RELEASE AND ASSIGNMENT
For good and valuable consideration, the receipt and legal sufficiency of which is hereby acknowledged, I ("I", "me", "my") hereby agree as follows:
1) I hereby grant to Warren Tattersall, his successors, assignees and licensees the unlimited right, but not the
obligation, to use any statements made by or attributed to me (my "Statements") as well as my name, voice, and likeness, performance, personal characteristics and other identifying information (jointly and severally with the Statements and the photographs referenced in Paragraph 2 below, my "Personal Characteristics") in and in connection with the advertising, promotion, marketing and other exploitation of Herbalife products or Warren Tattersall’s services in any and all languages and media, now known or hereafter devised, throughout the universe in perpetuity.
2) If I supply Warren Tattersall with photographs of myself on this date or any date subsequent, I agree that Warren Tattersall may use such photographs to the full extent provided above, I warrant and represent that I am the person depicted in the photograph, I am the owner of the photograph, I have the authority to grant the permission and rights granted herein, and no one else’s permission is required to grant such rights, and I understand that the copy of the photograph(s) I supply to Warren Tattersall will not be returned.
3) I understand that Warren Tattersall is not obligated to use my Personal Characteristics as permitted herein or, if commenced, to continue with such use in any territory. I acknowledge and agree that Warren Tattersall may make my Personal Characteristics available to Warren Tattersall’s independent distributors to use as permitted above.
4) In undertaking the act of submitting my words and images through www.TheHealthSuccessSite.com I understand that I am agreeing the terms and conditions of this agreement
I have read this entire General Release and Assignment and fully understand his contents. I likewise understand that this document shall remain in full force and effect unless/until I request that it be terminated, and that any such request must be made in a signed writing. By signing below, I hereby acknowledge and agree to the
foregoing.
I understand that in submitting my material for publication I am granting the rights to reproduce this material on the internet or in other form and I have read the conditions above
============================================================
SITE DISCLAIMER: Do these products “cure” anything? Of course not… but it stands to reason that if you cleanse your body and feed it the finest nutrition available, giving it everything it needs in balance, on a daily basis, that your body will do what nature intended, and give you the best possible chance to fend off sickness and disease. This Systemic Lupus Erythematosus your health online information is not presented by a medical practitioner and is for educational and Systemic Lupus Erythematosus informational purposes only. The Systemic Lupus Erythematosus content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any Systemic Lupus Erythematosus questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read. Any natural and/or dietary supplements that are not FDA approved or evaluated must be accompanied by a two-part disclaimer on the product label: that the statement has not been evaluated by FDA and that the product is not intended to "diagnose, treat, cure or prevent any disease”.
The Systemic Lupus Erythematosus resources on this your health online site are not intended to be a substitute for professional advice. While all attempts have been made to verify Systemic Lupus Erythematosus information provided in this publication, neither the author nor the publisher assumes any responsibility for errors, omissions or contrary interpretation of the web site Systemic Lupus Erythematosus subject matter herein. The what is Systemic Lupus Erythematosus your health online site Systemic Lupus Erythematosus contents are solely the opinion of the authors and should not be considered as a form of advice, direction and/or recommendation of any kind. If expert advice or counseling is needed, services of a competent professional should be sought. The what is Systemic Lupus Erythematosus author and the Publisher assume no responsibility or liability and specifically disclaim any warranty, express or implied for any Systemic Lupus Erythematosus products or services mentioned, or any techniques or Systemic Lupus Erythematosus practices described.
The purchaser or reader of this Systemic Lupus Erythematosus publication assumes responsibility for the use of these Systemic Lupus Erythematosus materials and your health online information. Neither the Systemic Lupus Erythematosus author nor the Publisher assumes any responsibility or liability whatsoever on the behalf of any purchaser or reader of these Systemic Lupus Erythematosus materials. There is no guarantee of validity of accuracy. This your health online website and its creators are not responsible for the content of any sites linked to
===========================================================